R.S. Regina Maris Hospital
With the help of Dr. Edward Muljadi, I recently completed a two-week medical internship in Medan, Indonesia, where I had the opportunity to shadow a doctor and gain real-world experience in patient care. From observing clinical procedures to learning how to communicate with patients, this experience gave me a deeper understanding of the medical field and strengthened my passion for healthcare.
Clinical Rounds
Dr. Edward makes a follow up visit for a woman 3 days after her C-section surgery. Before examining the wound, he disinfects his hand and then checks the wound where she had surgery. The only complaint she had was minor pain in her stomach. The doctor then determined that the condition is normal so he doesn’t prescribe any more medication.
Dr. Edward moves on to his next patient in a private ward. The patient said that she has burning pain from the stitches and pain from the tissue tumor in her finger. He then examines and treats the finger, and he tells her not to cover it up with bandages to prevent bacterial growth
The doctor then follows up with another patient who just delivered her baby. He checks the wound from the C section using his hand to see if it dried.
After the rounds, he documents patient conditions, complaints, and information in the computer in the Electronic Medical Record. He then gives the nurses instructions to help the patients
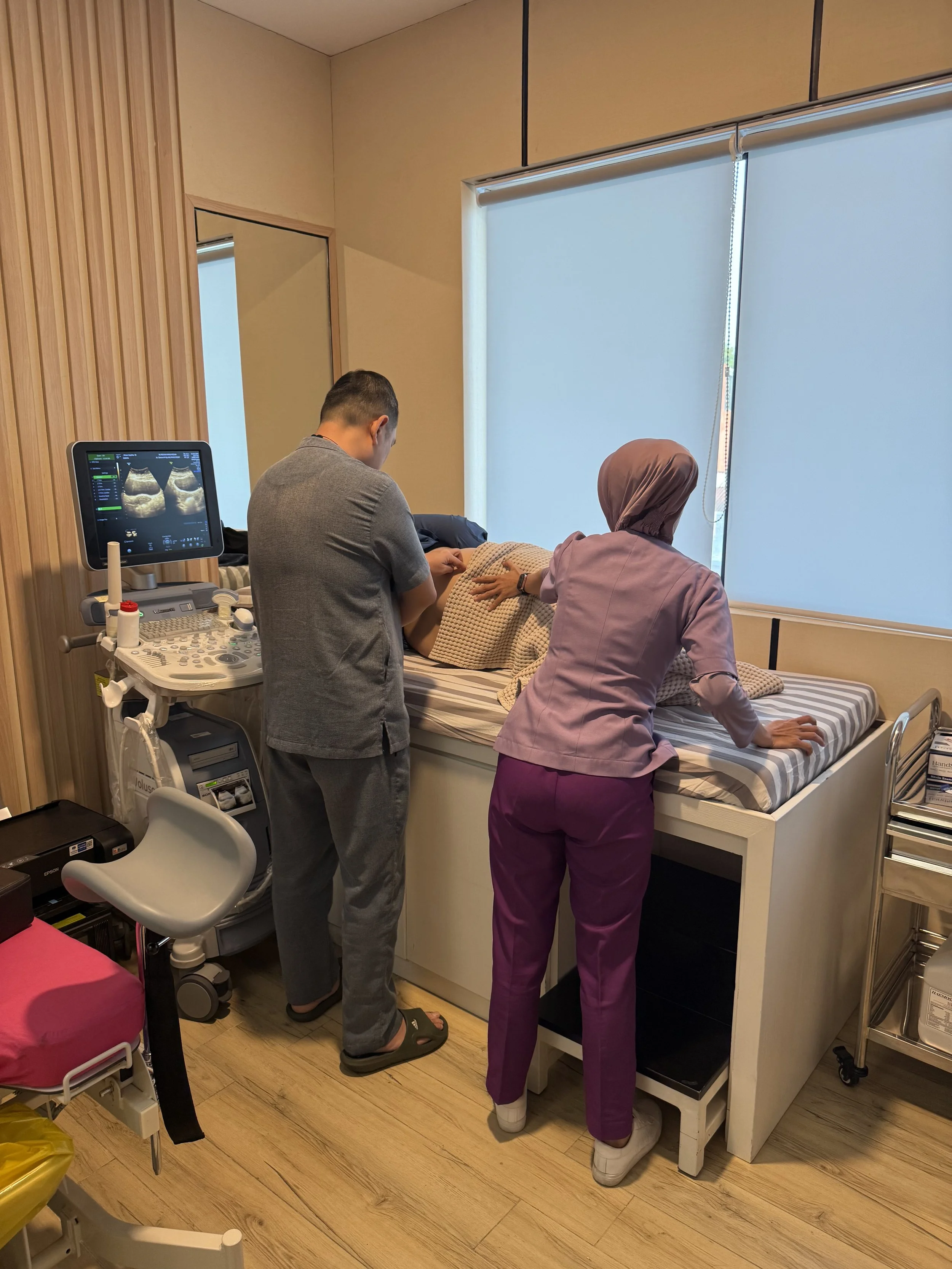
A pregnant woman complained about uncomfortable pain in her abdomen. The doctor then used an ultrasound to scan the baby, and it shows that she is 31 weeks pregnant. He concluded that she is experiencing pain because the baby is growing bigger. He then suggested that she could switch the position of the baby to decrease pain.
Dr. Edward follows up with a patient who just had a laparoscopic surgery to remove the growth of a tumor. To examine and change the dressing of the wound, he sprays his hand with alcohol first to disinfect it. The patient had C-section for deliveries earlier. Now she just went through laparoscopic surgery to remove the tumor.
The doctor then moves on to his next patient, who had fibroids growth. He recommends that she should use injections first to suppress the growth. After 3 months, she will do another follow up to check the size and growth and if the injections dont work, then keyhole surgery would be necessary to remove the fibroids.
The doctor then does a monthly pregnancy checkup with a new patient. By using the ultrasound, he can determine the age and gender of the baby.
Vendor communication: discontinue use of medical device from the vender because he had issues with it during the laparoscopic surgeries. He will decide to use another brand. As a result, the vendor will try to listen to the doctor’s concerns and will try to improve it.
Outpatient clinic
Surgery Shadowing
A laparoscopy is a type of minimally invasive surgery that allows doctors to look inside the abdomen or pelvis without making large cuts. It’s done using a thin tube called a laparoscope, which has a camera and light at the end. The surgeon makes one or more small incisions and inserts the laparoscope to view the internal organs on a screen. This procedure is often used to diagnose or treat problems like ovarian cysts, endometriosis, fibroids, or unexplained pain in the lower abdomen.
If treatment is needed, the surgeon makes one or more additional small cuts in the abdomen to insert surgical tools. These tools allow the doctor to remove tissue , take samples, or fix any problems. Once the procedure is done, the instruments and gas are removed, and the small incisions are closed with stitches or surgical tape. Most patients can go home the same day and recover much faster compared to open surgery, with less pain and minimal scarring.
After the doctor viewed this patient’s organs, he discovered that a bigger fibroid was covering up smaller fibroids that were spread out on the ovary. The laparoscopy procedure was ineffective against bigger sizzed fibroids. As a result, he had to move on to a different surgical procedure in order to remove the bigger fibroid.
During a laparoscopy, the patient is first placed under general anesthesia, so they are asleep and won’t feel pain during the procedure. Once the patient is asleep, the surgeon makes a small incision near the belly button. Through this opening, a thin tube called a laparoscope—which has a tiny camera and light—is inserted. The abdomen is then filled with a harmless gas, usually carbon dioxide, to gently inflate the area. This gives the surgeon more space to see and work, as well as a clearer view of the internal organs on a video monitor.
Public Work
After completing his shift at a private hospital, Dr. Edward volunteered his time and skills at a nearby public hospital, where medical resources and staff were often limited. Despite the long hours of his regular workday, he made it a priority to give back to the community by assisting with surgeries that required extra hands. He joined the surgical team in performing a laparoscopic procedure, which helped reduce the workload on the overburdened staff and ensured the procedure could be done more efficiently and safely.
As the lead surgeon, the doctor carefully handled the instruments and monitored the internal camera feed in order to perform the surgical procedure. As a result, the public hospital team appreciated his commitment, especially since patients in underfunded hospitals often wait longer for treatment. His willingness to volunteer not only improved the care for that patient but also reflected the deep sense of responsibility many doctors feel toward those in need, regardless of where they work.
Interview Q&A
a. What does your job as a doctor involve?
As an OB-GYN with subspecialty training in gynecological endoscopy, I provide comprehensive women’s healthcare. This includes prenatal care, childbirth management, cancer screenings (e.g., Pap smears), family planning, and treating conditions like endometriosis, fibroids, and infertility. My endoscopic expertise involves minimally invasive procedures such as hysteroscopies (examining/treating the uterus) and laparoscopies (keyhole surgery for cysts, adhesions, or ectopic pregnancies), which reduce recovery time and complications compared to open surgery.
b. What motivated you to become an OB-GYN doctor?
I was drawn to the unique blend of surgery, long-term patient relationships, and the ability to impact women’s lives during pivotal moments—whether delivering a baby, managing menopause, or diagnosing a life-changing condition. The field merges technical skill with profound human connection.
c. What are some common health problems women face?
- Reproductive age: PCOS, endometriosis, fibroids, infertility, STIs.
- Pregnancy: Gestational diabetes, preeclampsia, preterm labor.
- Midlife/Later: Menopausal symptoms (hot flashes, bone loss), pelvic organ prolapse, breast/ovarian/uterine cancers.
- Universal issues: Mental health (e.g., postpartum depression), urinary incontinence, and gender-based violence impacts.
d. What does a typical day look like?
My days are unpredictable but generally include:
- Mornings: Endoscopic surgeries (e.g., laparoscopic myomectomies).
- Afternoons: Clinic appointments—prenatal checks, post-op follow-ups, cancer screenings.
- Nights/Weekends: On-call emergencies (e.g., ectopic pregnancies, deliveries). I often work 12–16 hours/day, with sleep interrupted by urgent calls.
e. What is the most rewarding part of being an OB-GYN?
Empowering women through transformative care: handing a mother her newborn, ending years of pain via endometriosis surgery, or guiding a cancer survivor to remission. These moments reaffirm why I endure the demanding schedule.
f. What are the biggest challenges?
- Work-life imbalance: High emergency volume makes rest/leaves scarce.
- Emotional toll: Managing obstetric complications (e.g., stillbirths) or terminal diagnoses.
- Systemic issues: Administrative burdens, insurance limitations, and societal gaps in women’s health access.
g. How has your approach to patient care evolved?
I’ve shifted from paternalistic to patient-centered .I prioritize listening, explaining options in plain language, and respecting cultural/autonomy preferences—especially in sensitive areas like fertility or sexual health.
h. How does teamwork play a role?
It’s essential. I collaborate with:
- Midwives/Nurses: For prenatal care, deliveries, and patient education.
- Oncologists/Radiologists: For complex cancer cases.
- Embryologists: In IVF treatments.
Trust and communication within this team save lives daily.
i. How do you help patients feel comfortable?
- Before procedures: Explain each step, show instruments, and discuss pain management.
- During exams: Use drapes for privacy, offer a chaperone, and check in frequently.
- Cultural sensitivity: Use inclusive language, acknowledge religious/personal beliefs, and never rush them.
j. What qualities are vital for success?
- Resilience: To handle physical/emotional demands.
- Empathy: To connect with patients in vulnerable moments.
- Adaptability: For evolving science and unexpected crises.
- Surgical precision: Especially in endoscopic work.
k. Advice for an aspiring pre-med student?
1. Shadow doctors (especially OB-GYNs) to experience the reality.
2. Develop bedside manner early Volunteer in women’s shelters or clinics.
3. Prioritize self-care Medicine is a marathon—build healthy habits now.
4. Stay curious Women’s health is rapidly advancing (e.g., fertility preservation, genomic medicine).